In recent times myopia management has attracted significant interest from researchers and eyecare practitioners, with representative bodies such as the World Council of Optometry calling for myopia management to be part of the standard of care for myopic patients (1). The public is also becoming more aware of myopia management and the complications associated with developing worse myopia. There are now a number of myopia management options available to eyecare practitioners which can be tailored to individual patients’ needs and circumstances. Orthokeratology (ortho-k) is one such option supported by a significant body of evidence and has the added advantage of providing excellent unaided vision during the day.
.png)
Author: Michael Moore
20 June 2022
Orthokeratology for Myopia Control
Orthokeratology
Doctor George Jessen first described the procedure for fitting ortho-k lenses in 1962. The process involved fitting a series of progressively flatter-fitting rigid lenses worn during the day. Over time, this would result in the flattening of the central cornea and the reduction of myopia. Unfortunately, this method of ortho-k fitting provided highly variable results and did not gain widespread popularity. Several innovations in the last decades have meant that most problems originally associated with ortho-k fitting have been overcome. Lens materials that provide high oxygen transmission allow lenses to be worn safely overnight, resulting in lens-free corrected vision during the day. Reverse geometry designs provide easier fits, more predictable results and quicker improvements in vision, while corneal topography allows more accurate pre-treatment assessment and post-treatment monitoring and adjustment.

Fluorescein pattern and cross-sectional representation of a reverse geometry orthokeratology lens. A represents the flat base curve, B represents the reverse curve, C represents the alignment curve and D represents the peripheral curve. Reproduced from Nti and Bersten(2).
Myopia Control
Orthokeratology has been investigated as a form of myopia management since the mid 2000s. However, as far back as 1957, there have been reports of the reduced myopia progression associated with flat-fitting rigid contact lenses, which could be considered analogous to ortho-k. The mechanism by which ortho-k lenses provide their myopia control effect is thought to be the induced peripheral defocus that occurs after a successful treatment. This is similar to the mechanism by which most soft peripheral defocus contact lenses are thought to provide myopia control.
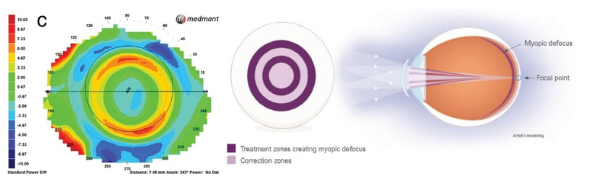
Comparison of a corneal topography difference map (pre-treatment – post-treatment) from a treated orthokeratology patient with a MiSight soft contact lens treatment zone schematic. Both are thought to reduce myopia progression as they both provide peripheral myopic defocus. Reproduced from Nti and Bersten.2
Numerous studies have reported the efficacy of ortho-k as a myopia management option. The reported statistics of any study describing the efficiency of a myopia management strategy need to be interpreted carefully. For example, a five year follow up of Japanese children treated with ortho-k for myopia control found a 31% reduction in axial elongation in the treated children when compared to control. (3) The effect was more significant for the initial three years than the final two years, which the authors suggest is due to the natural reduction of axial length elongation that occurs with age. This means that the level of myopia control achievable in an individual patient will not always tally with reported results due to differences in age, level of myopia etc. Most studies comparing ortho-k lenses to control groups demonstrate an approximately 30-60% reduction in myopic progression(4), with a meta-analysis showing a reduction of axial length elongation of 0.25-0.27 mm over two years in children using ortho-k lenses. (5,6)
Patient Selection and Fitting Procedure
Most modern orthokeratology designs can correct up to approximately 5.00 dioptres of myopia and about 2.00 D of astigmatism. Patients with myopia exceeding these levels can sometimes be successfully fit with ortho-k lenses. However, it becomes more challenging to achieve a good result with higher attempted corrections. Patients with very large pupils are also contraindicated due to the possibility of symptoms resulting from higher order aberrations. All other typical requirements for successful contact lens wear should also be met.
The typical schedule of appointments used for ortho-k patients is an initial assessment, including vision and refraction, slit-lamp exam, and topography. If the patient is interested in ortho-k for myopia management, we also have an in-depth discussion on all the available options that would most suit the patient. If the patient is suitable, lenses are ordered based on the topography and refraction findings at this stage. During the follow-up consultation, the eyecare professional uses fluorescein to assess the lens on the eye and the patient is instructed on handling the lens. The patient then needs to attend early in the morning after wearing the lens overnight for the first time. They usually attend with the lens still in situ and it is again assessed on the eye with fluorescein. The clinician can then remove the lens, ensuring there are no issues with lens binding. The patient then has a vision and refraction assessment along with topography. Usually, after just one night of wear, treatment effects will be apparent and improvements of 50-70% in refraction and vision are not unusual. At this point, it can be useful to use daily disposable contact lenses to correct any residual refraction if appropriate.
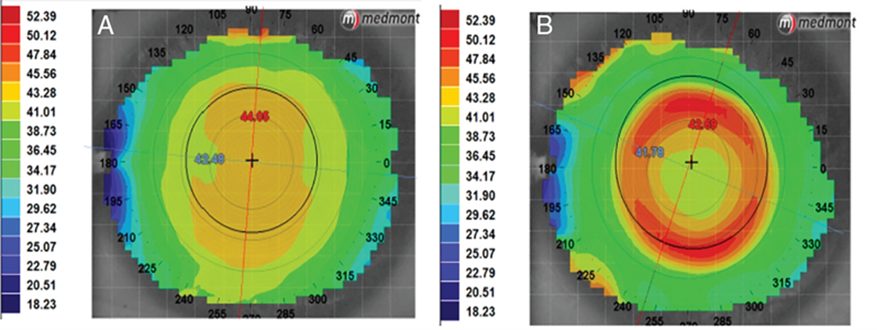
Pre-treatment (A) and post-treatment (B) corneal topography of an orthokeratology patient. Topographical changes will be apparent after just one night of wear.
After one week, the above appointment is repeated and the patient has usually achieved close to a complete correction. A final appointment is usually required after one month of wear, with this appointment taking place later in the day with no lens in situ. This is to determine that the treatment is lasting throughout the day. As ortho-k is a reversible procedure, some patients may notice a regression in the treatment effect throughout the day. As can be seen, there is more chair time required with fitting ortho-k than a typical soft contact lens. This should be discussed with the patient so they understand this commitment and any additional cost implications.
Safety of Orthokeratology
There have been several investigations into the safety of ortho-k fitting, particularly due to its use in paediatric populations as myopia management. The rate of complications that arise from the use of ortho-k lenses in children ranges from approximately 11-13%, similar to soft contact lenses. The vast majority of these complications are considered non-significant and do not require the cessation of lens wear. (7, 8) The most common complication encountered in our clinic is mild central corneal staining which usually does not require intervention. There is a risk of developing microbial keratitis (MK) with any form of contact lens. Due to the low numbers of patients using ortho-k lenses and low incidence of MK, it is difficult to accurately compare the rates of MK in ortho-k lens wearers to soft lens wearers. However, ortho-k does appear to convey a higher risk (4). It is essential to discuss these risks with patients before commencing lens wear, pondering the risk of increasing myopia levels when ortho-k is used for myopia management. It has been demonstrated that the lifetime risk of vision impairment due to myopia far exceeds the lifetime risk of vision impairment due to MK from ortho-k lens wear. (9)
As myopia management becomes the standard of care for all new myopic patients, we must have a range of options that will suit each individual patient’s needs. Orthokeratology is one such option and practitioners should consider its potential for all young myopic patients.
Ocuco is a leading supplier of professional eyecare software and software for family run opticians as well as larger chain opticians.
Ocuco offers innovative eyecare software, designed for independents, chains, and labs. Whether you need optical retail shop software for your independent optical retail shop, optical chain software to manage a chain business or optical lab management software for your lab, we have the ideal solution for your optical needs.
Are you looking for optical practice management software ? Acuitas offers product management, electronic health record systems, appointments and multiple configurations to meet the specific needs of your optical business. Contact us today for free expert advice!
Additional Reading
- Folkesson P. The Standard of Care For Myopia Management by Optometrists. World Council of Optometry Resolution. Published 2021. https://worldcouncilofoptometry.info/resolution-the-standard-of-care-for-myopia-management-by-optometrists/
- Nti AN, Berntsen DA. Optical changes and visual performance with orthokeratology. Clin Exp Optom. 2020;103(1):44-54. doi:10.1111/cxo.12947
- Hiraoka T, Kakita T, Okamoto F, Takahashi H, Oshika T. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: A 5-year follow-up study. Investig Ophthalmol Vis Sci. 2012;53(7):3913-3919. doi:10.1167/iovs.11-8453
- Vincent SJ, Cho P, Chan KY, et al. CLEAR – Orthokeratology. Contact Lens Anterior Eye. 2021;44(2):240-269. doi:10.1016/j.clae.2021.02.003
- Sun Y, Xu F, Zhang T, et al. Orthokeratology to control myopia progression: A meta-analysis. PLoS One. 2015;10(4):1-9. doi:10.1371/journal.pone.0124535
- Wen D, Huang J, Chen H, et al. Efficacy and acceptability of orthokeratology for slowing myopic progression in children: A systematic review and meta-Analysis. J Ophthalmol. 2015;2015. doi:10.1155/2015/360806
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Orthokeratology vs. spectacles: Adverse events and discontinuations. Optom Vis Sci. 2012;89(8):1133-1139. doi:10.1097/OPX.0b013e318263c5af
- Hiraoka T, Sekine Y, Okamoto F, Mihashi T, Oshika T. Safety and efficacy following 10-years of overnight orthokeratology for myopia control. Ophthalmic Physiol Opt. 2018;38(3):281-289. doi:10.1111/opo.12460
- Bullimore MA, Ritchey ER, Shah S, Leveziel N, Bourne RRA, Flitcroft DI. The Risks and Benefits of Myopia Control. Ophthalmology. 2021;128(11):1561-1579. doi:10.1016/j.ophtha.2021.04.032

Doctor Michael Moore is a lecturer, researcher and Clinical Supervisor with the School of Physics and Clinical and Optometric Sciences at Technological University Dublin (TUD), Ireland.
Dr Moore carries out his research as part of the Centre for Eye Research Ireland (CERI), primarily focusing on myopia, epidemiology and Big Data. Dr Moore also supervises clinics in the National Optometry Centre and mainly concentrates on complex contact lens fitting.