Crucially, scientific and industrial innovators have responded to the threat posed by myopia. We now have a rapidly increasing range of treatments available which have been shown to delay myopia onset, reduce or eliminate the progression of myopia in some children and which may thereby reduce the risk of long term damage. Consequently, we have reached a stage where progressive myopia is no longer just a refractive state, but is now considered a modifiable risk factor for the development of eye disease and associated vision loss.
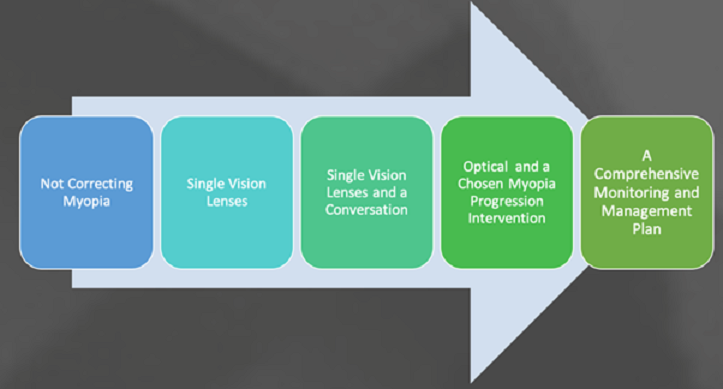
Myopia management has become one of the most dynamic and fast-changing areas of ophthalmic clinical practice. The question now arises as to what exactly is the standard of care for myopia management. The release of Myopia Management Guidance for Optometrists from the UK College of Optometrists, somewhat controversially stated that “the evidence is not sufficient to recommend the wide-scale roll out of any myopia control intervention”. This has undoubtedly contributed to the general indecisiveness among some practitioners about making the transition from passive to active myopia management. More recent developments, however, are likely to resolve any lingering reluctance to engage and should fast track the transition to proactive rather than reactive myopia care.
What do we mean by “Standard of Care”?
According to the New England Journal of Medicine (2004), Standard of Care is defined as “a diagnostic and treatment process that a clinician should follow for a certain type of patient, illness, or clinical circumstance”. As clinicians, however, we also need to be cognisant of its legal as well as clinical meaning, because the standard of care is critical in terms of establishing medical malpractice/negligence. From a legal perspective, standard of care does not mean perfection in practice but instead requires that a practitioner should exercise the degree of skill, care and learning possessed by others in the same profession.
Scientifically robust clinical practice guidelines can be used to define the standard of care, but they do not necessarily set the legal standard. One important consideration is that customary practice, i.e. what is commonly done, may not be considered enough. So although it has been customary to simply correct myopia with traditional methods, this may not provide protection in any legal action. Practitioners should instead be seen to take all “reasonable” measures in the care they provide for their patients.*
World Council of Optometry Resolution: The Standard of Care for Myopia Management by Optometrists
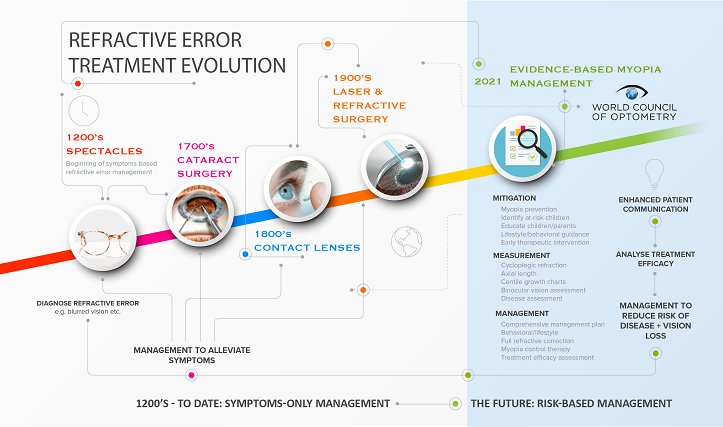
In April 2021, the World Council of Optometry (1) called for a new evidence-based standard of care for myopia management by optometrists, comprising three main components, the 3 M’s:
- Mitigation – as optometrists, we should appropriately educate and counsel parents and children, discuss risk factors and provide lifestyle/behavioural guidance during early and regular eye exams. Such measures allow us to contribute to the prevention/delayed onset of myopia or facilitate early detection and therapeutic intervention.
- Measurement – optometrists should comprehensively evaluate the status of a patient during regular vision and eye health exams including refractive error and axial length measurement (whenever possible).
- Management – optometrists should address patients’ needs of today by correcting myopia while also providing evidence-based interventions (e.g. contact lenses, spectacles, pharmaceuticals, behavioural guidance) that slow the progression of myopia, for improved quality of life and better eye health today and into the future.
This resolution recognises the pivotal role optometry can play as a profession, specifically targeting the continued reluctance of some optometrists to integrate the increasing scientific evidence relating to myopia control into their clinical practice. Importantly, the resolution states that the lack of an appropriate standard of care for myopia management is a disservice to the optometry profession, our patients and public health.
.png)