Author: Tania Constable
23 October 2024
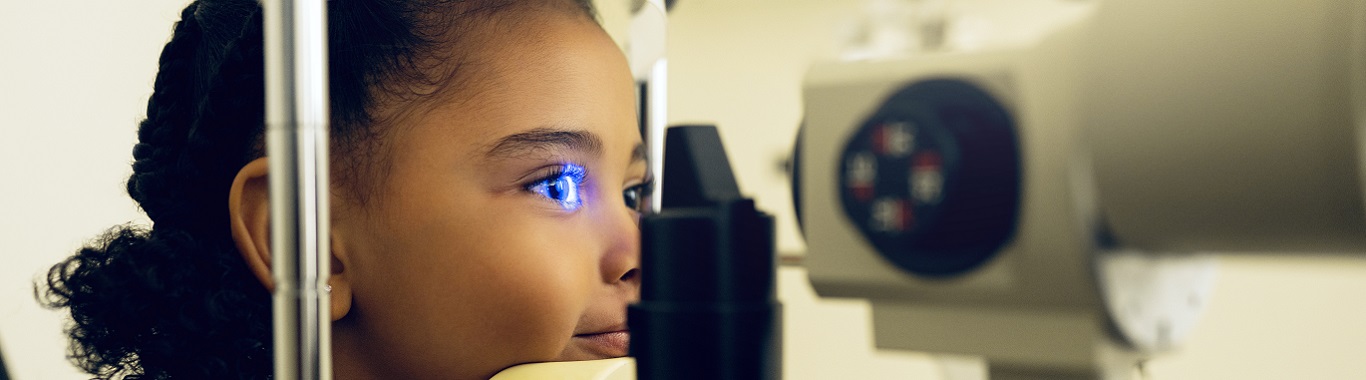
ABCs for Children’s Eyecare
In the UK and Ireland while school-aged children undergo vision screening for amblyopia at enrolment, this alone is insufficient. Visual acuity in young children is a poor predictor of refractive error, especially in young hyperopes. Vision is crucial for development, playing a role in speech development and motor skills.
It goes without saying that good vision is critical for education. All parents should be encouraged to have their children’s eyes examined. The most common conditions managed in paediatric clinics include refractive error, strabismus, and amblyopia. Parents may also express concerns about watery eyes, blepharitis and some visual behaviours, such as excessive blinking or proximity to screens.
Effective paediatric eyecare requires a comprehensive approach. In addition to early detection and treatment of conditions like amblyopia and refractive errors, creating a child-friendly environment and utilising age-appropriate communication techniques are essential. By fostering a positive and supportive atmosphere, healthcare providers can build trust and ensure accurate assessments, leading to optimal outcomes for young patients. We will discuss these aspects in more detail below.
Environment
Having a child-friendly space is important for paediatric eyecare. Consider the space from a young child’s perspective. Cover scary-looking equipment, and pack away as much of the equipment as possible. Allowing movement breaks helps children stay on task. Having accessible toys can help during discussions with parents about management plans. Pop friendly cartoon characters like Bluey on the windows and doors. Remember, some children fear the dark so having night lights on the room can also help.
Communication
Be tuned into nonverbal communication such as body language. Avoid the use of nuances or colloquial phrases, use literal direct language. Don’t provide too much information at once and in different
ways as this is confusing for younger children.
Visual Acuity Testing
It is important to use the age-appropriate test for the child. A crowded visual acuity test is important for children under 8 years old to detect amblyopia. Record the visual acuity measured in LogMAR where possible. For children under the age of 2 years, preferential looking tests like the Cardiff visual acuity cards are ideal.
Information to always record when measuring visual acuity in children:
- Which test was used
- Testing distance
- Which eye was measured first
- Whether a matching card was used or the naming of the target
- If the child was shy or reticent
Refractive Status
It is advisable to carry out a baseline cycloplegic refractive on all children. Objective tests such as retinoscopy are invaluable for younger children. In addition to providing an objective measure of the refractive error, the quality of the reflex can also provide information on ocular health, such as the presence of any lens opacities.
Other useful retinoscope techniques include Mohindra (for non-cycloplegic retinoscopy) and dynamic retinoscopy, which is a useful technique to gauge the accommodative function and, therefore inform prescribing.
To Prescribe or not to Prescribe?
Factors to consider before prescribing include:
- Is the visual acuity reduced?
- Is the refractive error within the normal range for the age?
- Is the child symptomatic?
- Are there any accommodative deficits?
- Is there a strabismus? Or binocular vision issues that can be refractively managed such as amblyopia
Visual acuity varies depending on the visual acuity test used. Cardiff visual acuity cards, Kay pictures visual acuity test and Sonksen acuity test all have normative values based on age.
The distribution of refractive error varies depending on the child’s age and can be broadly divided into under 6 years of age and over 6 years of age. When deciding whether to prescribe or not, it is important to consider if the refractive error is normal for the age, for example a 2-year-old with -2.50DC of astigmatism doesn’t require correction. The RCOph considers refractive error greater than +3.50 to +4.00DS an amblyopic risk factor. Anisometropia greater than 1.00D should be managed refractively.
Under the Age of 6
The mechanism of controlling eye growth drives refractive error towards low hyperopia or emmetropia. The largest changes in refractive error occur before the age of 6; the changes in spherical refractive error occur independently of astigmatic changes. There is a shift from +2.00DS towards +0.75DS. It is unusual to find myopes under the age of 4-5 years, and if this occurs, further investigation would be advisable.
Over the Age of 6
Most emmetropisation is complete by the age of 6, and this is when the incidence of myopia tends to increase. Historically, most children at 6 years old were still hyperopic, but given the wave of little myopes, it is not uncommon to encounter 6-year-old myopes; the challenge here is that myopes are becoming myopic within their critical period of visual development.
Ocular Health
You don’t commonly encounter ocular health issues in children’s eye clinics. Some conditions that may be encountered include:
- Blepharitis
- Developmental cataracts
- Keratoconus
- Retinal dystrophies
- Albinism
Amblyopia Management
Amblyopia is the most common cause of visual impairment in children and can affect one or both eyes. Anisometropic amblyopia can be easily managed refractively. Children should be reaccessed after 4 months of refractive adaption. Occlusion therapy in the presence of esotropia should be managed in accordance with the PEDIG guidance.
Ocular Health
Serious ocular health issues are not common in children's eye clinics. Conditions that can be encountered include:
- Keratoconjunctivitis
- Developmental cataracts
- Keratoconus
- Retinal dystrophies
- Albinism
Top tips
- Have rewards such as stickers for each step along the way
- Include the child in the history and symptoms for early engagement
- Be flexible and consider a need-led approach

Tania Constable is a full-time paediatric specialist optometrist, working in both a primary and secondary care setting in Dublin.
Tania holds Paediatric Eyecare, Glaucoma and Medical Retina certificates from the College of Optometrists and an MSc in Clinical Optometry from Cardiff University. She has experience working with children with additional needs, such as Autism Spectrum Disorder (ASD) and Down’s Syndrome, and raising awareness of the difficulties associated with cerebral visual impairment. Tania currently serves as the president of Optometry Ireland.