In The Global Impact of COVID-19 on Eyecare and Eye Health – Part 1, we explored how the COVID-19 pandemic and associated safety measures have restricted access to eyecare and prompted rapid changes in the provision and delivery of eye health services worldwide. The evolution of clinical services may benefit patients in the long term, but as the pandemic continues into its second year, it is worth exploring areas in which COVID-19 may have led to an adverse direct or indirect impact on ocular health.
.png)
Author: James Loughman
26 April 2021
The Global Impact of Covid-19 on Eyecare and Eye Health - Part 2
Direct effects of COVID-19 on the eye
According to a recent meta-analysis of published studies, approximately 11% of COVID-19 patients have exhibited direct ocular effects (1). Typically, the complications appear to be relatively mild and short-term. The most common ocular manifestation of COVID-19 infection is unilateral or bilateral conjunctivitis (typically viral), while ocular pain, dry eye, floaters, eyelid dermatitis and keratoconjunctivitis have also been reported. A study from Anglia Ruskin University has found that sore eyes appear among the most commonly reported symptoms of COVID-19 and that ocular symptoms manifest simultaneously to other COVID-19 symptoms.
The treatment of patients with severe complications of COVID-19, which required prolonged prone-position ventilation, has led to some more serious ocular complications. Case studies have been published relating to ICU patients who developed significant periorbital edema, two of whom also developed orbital compartment syndrome (increased IOP of 2- to 3-fold in prone positioning) and papillophlebitis (optic disc elevation with associated hemorrhages) following four to nine 18-hour ventilation sessions in the prone position.
Indirect effects of COVID-19 on the eye
The indirect effects of COVID-19 are much broader and relate to various causative factors, including service delays, lifestyle and behavioural changes and psychosocial impacts. While the long-term ocular health and quality of life impact of COVID-19 will be challenging to quantify, significant concerns exist. Some evidence has started to emerge, which clinicians may need to address in the post-COVID pandemic period.
"Case studies have been published relating to ICU patients who developed significant periorbital edema, two of whom also developed orbital compartment syndrome."
Service delays and cancellations
Since COVID-19 emerged, lockdowns and concerns about virus exposure have caused cancellations and delays to routine appointments. These measures present a particular challenge in treating age-related conditions, given that the mortality from COVID-19 is highest in the age group of patients most likely to suffer eye disease. Treatment of neovascular age-related macular degeneration with vascular endothelial growth factor (VEGF) inhibitors therapy is an obvious example, as regular and frequent treatments are necessary for optimal outcomes in most patients. Delays in the care of new-onset and persistently active cases are a reality because the potentially life-threatening risk of COVID infection may outweigh the risk of recurrence and visual loss. How big this risk of visual loss is, and over what period it may manifest, remain unclear. Even after the lockdowns and risks of COVID have hopefully receded, waiting lists for care for this and other conditions such as cataracts and glaucoma will take time to address. They will inevitably lead to vision loss which may have a significant and lasting quality of life impact.
Lifestyle and behavior change
A new article of clothing has emerged in the past year, the face mask, which has also given rise to a new phenomenon known as Mask Associated Dry Eye (MADE). Widespread use of face masks, while essential for the prevention of novel coronavirus transmission, may cause ocular dryness and irritation due to increased airflow upwards from under the mask. This accelerates evaporation of the tear film and may result in ocular surface irritation or inflammation.
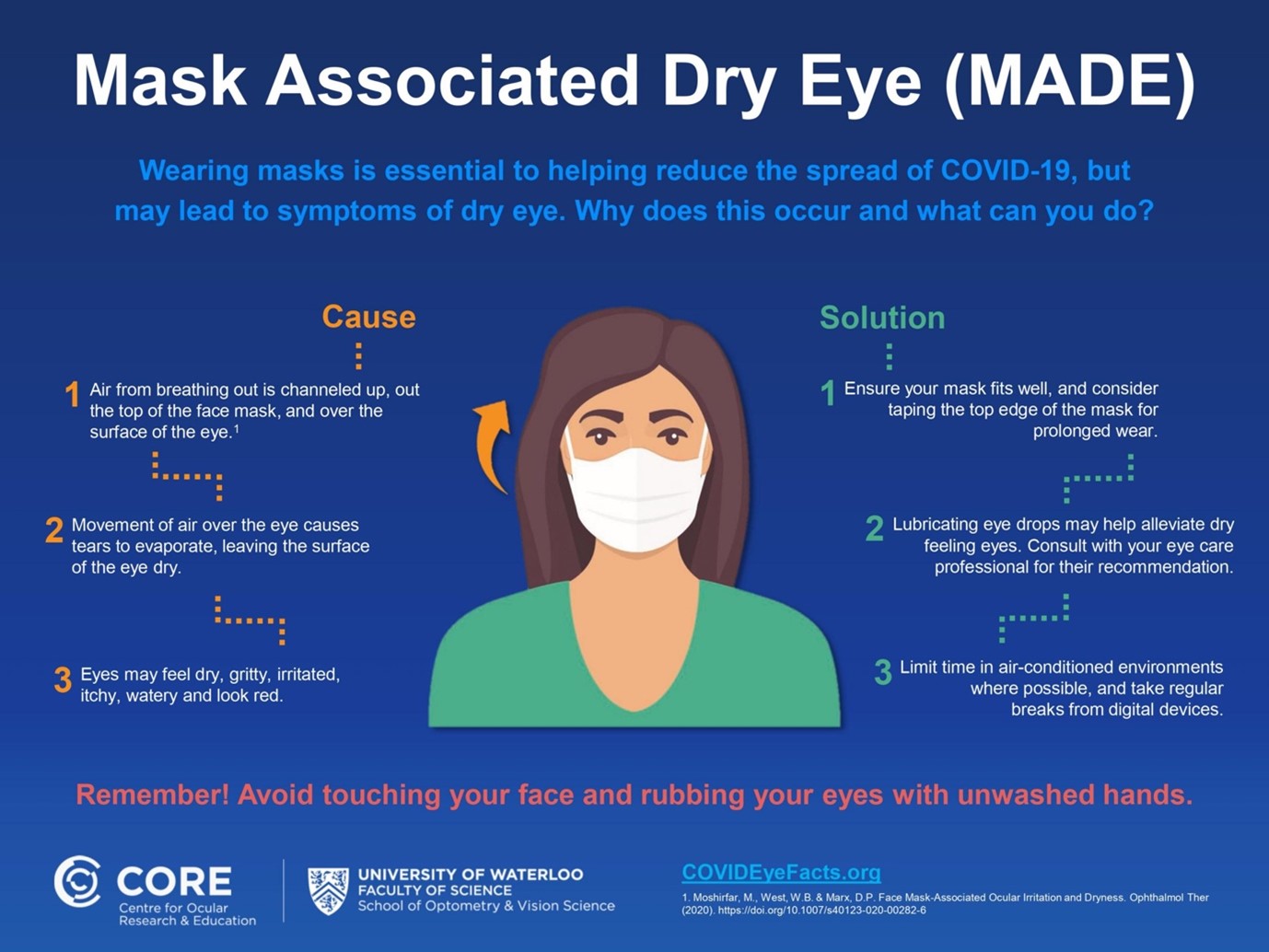
Experts from the Centre for Ocular Research & Education (CORE) are advising eye care professionals (ECPs) on how to recognize mask-associated dry eye (MADE) and
methods to mitigate the condition.
Increases in dry eye syndrome may also be a more general complication of prolonged screen time while learning or working from home. While readily treatable, the various possible COVID-related causes of dry eye need to be factored into the clinical eye examination in order to determine the appropriate guidance and treatment for individuals affected. The elderly, for example, typically have a poorer quality tear film, while contact lens wearers and masked people working extended hours in air-conditioned settings and/or while using digital screens may be particularly affected (3).
Growth in the rate of myopia represents another potential consequence of COVID-19 lockdowns and associated lifestyle changes. Increased screen time among children is an inevitable consequence of the switch to online learning, while lockdowns have likely restricted outdoor exposure and led to increased indoor leisure time spent using devices. A recent study from China (4) has shown that as a result of COVID-19 restrictions, myopia has increased dramatically, especially in younger children, seeing 2020 marked down as the year of “quarantine myopia”(5). In China, home confinement during the COVID-19 pandemic was associated with a substantial myopic shift for younger school-aged children (6-8 years). These children were up to 3 times more likely to become myopic compared to the previous 5 years. Table 1 highlights the significant increase in myopia prevalence in younger children in 2020 compared to earlier years. These changes in young children are worrying, given the risks of eye disease and vision impairment linked to myopia.
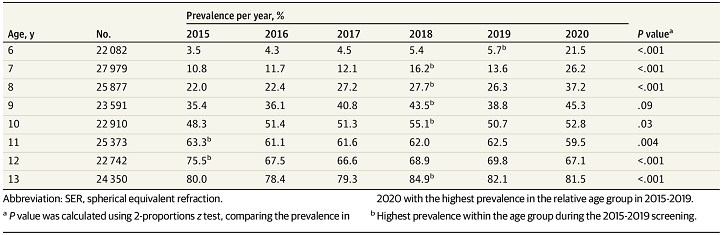
Table 1: Prevalence of myopia from 2015 to 2020 in school-aged children in China according to age.
Another study in China has just released additional data showing that the rate of myopia progression accelerated in children and teenagers during lockdown but subsequently reverted to pre-lockdown levels, suggesting that accommodative spasm may have been a factor in the acceleration. The combined evidence suggests that future lockdowns should be managed in a way that reduces the risk of myopia development or accelerated progression.
Psychosocial impact on patients with vision impairment
Another important consideration is the possible effect of COVID-19 lockdown on people with vision impairment who might be particularly vulnerable to the psychosocial impacts of the emergency measures deployed to counter the pandemic. A study in the UK has revealed that lockdowns led to anxiety, stress and fear among people living with vision impairment, negatively impacted mental health (45.9%), caused loneliness (46.0%), social life disturbances (85.3%), anxiety related to hospital visits (55.1%), and fear of further sight loss due to delayed review/treatment (45.9%). The lockdowns reinforced the limitations posed by participants’ vision impairment on undertaking routine activities or providing care to other family members. (Fig. 1).
Figure 1: Self-reported psychosocial impact on COVID-19 on people with vision loss (6)
One thing is for certain, COVID-19 will leave behind a long and lasting impact on eyecare services and eye health. While vision may not seem particularly important in comparison to the risk of death, it is critical to consider the impact of this global pandemic so that we can refine and improve future responses in ways that minimize the possible short and long-term impact on ocular comfort, eye health and vision-related quality of life. For now, as clinicians, we should be wary of how COVID-19 may have impacted our patients and endeavor to find solutions to reduce any long-term effects.
References:
1. https://iovs.arvojournals.org/article.aspx?articleid=2770655
2. https://bmjophth.bmj.com/content/5/1/e000632#aff-1
3. https://core.uwaterloo.ca/news/core-alerts-practitioners-to-mask-associated-dry-eye-made/
4. https://jamanetwork.com/journals/jamaophthalmology/fullarticle/2774808
5. https://jamanetwork.com/journals/jamaophthalmology/fullarticle/2774806
6. https://www.nature.com/articles/s41433-020-01130-4#Fig1
James Loughman is the Clinical Research Director for Ocuco Ltd.
An Optometrist with more than 20 years of clinical, academic, research and management experience, James recently joined Ocuco as Clinical Research Director. James is also presently the Director of the Centre for Eye Research Ireland, a research facility based in the Dublin Institute of Technology, the same university where he received his PhD in 1997; James oversees a portfolio of research including technology development and big data analytics projects alongside various clinical trials for the control of myopia, glaucoma and other blinding conditions.